By Dana Hudepohl,
Last Updated:In the United States, someone has a heart attack every 40 seconds. Every year, more than 800,000 Americans have a heart attack, and 320,000 have out-of-hospital cardiac arrests. Here, learn the difference between the two and what you can do to dramatically lower your risk for either. If you believe that you may be experiencing a heart attack or cardiac arrest, call 911 immediately.
Heart Attack vs. Cardiac Arrest
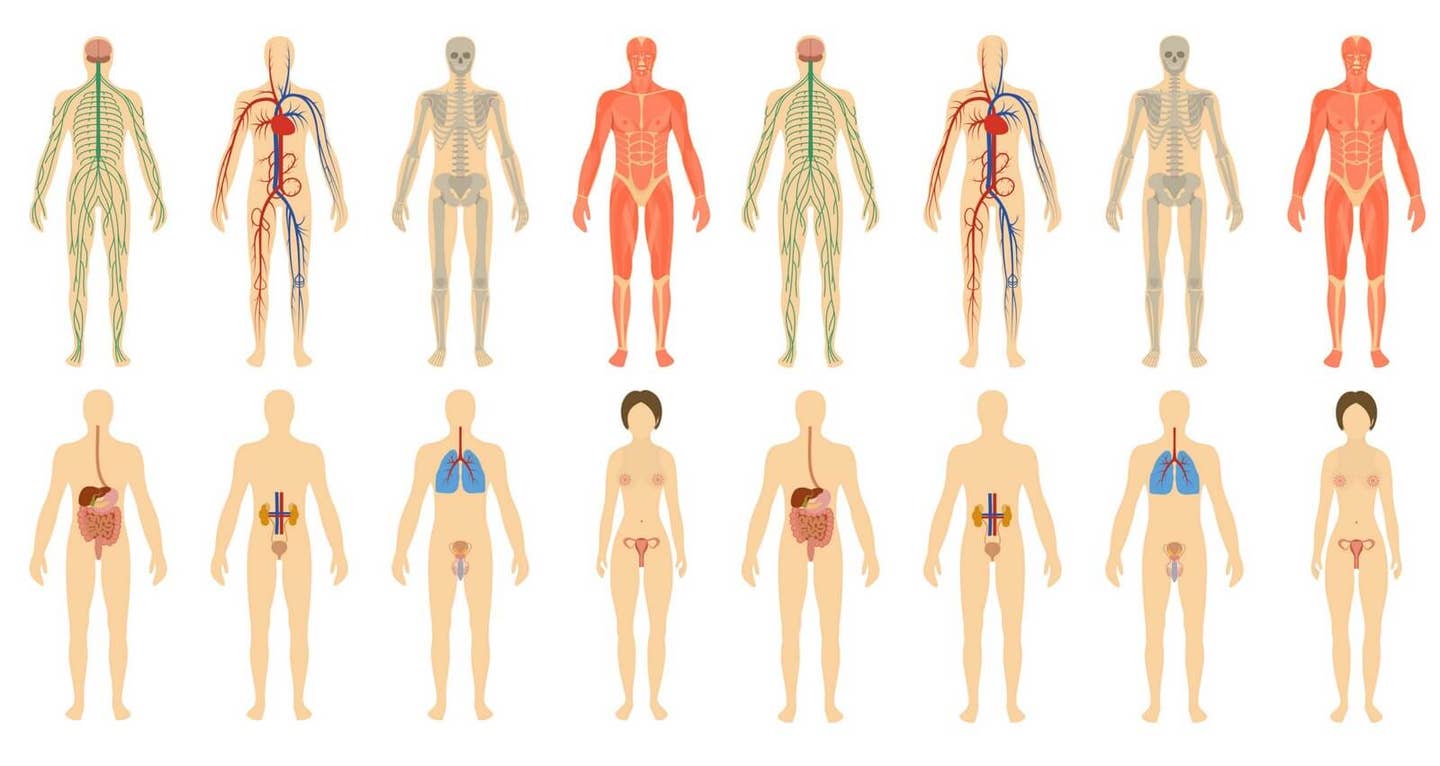
While both heart attack and cardiac arrest impact the heart muscle and are life-threatening, the terms describe different underlying mechanisms.
What Is a Heart Attack?
A heart attack (myocardial infarction) is a problem with circulation. “A heart attack affects the plumbing of the heart,” explains Columbus Batiste, MD, chief of cardiology at Kaiser Permanente Riverside Medical Center. “The blood supply to the heart muscle is reduced or blocked, leading to damage to the heart muscle, but the heart keeps beating.” The more time that passes before blood flow is restored, the more damage occurs to the heart. Heart attacks can be fatal, but survival rates have markedly improved over the past few decades, thanks to increased prevention efforts and advancements in treatment.
Complications that can arise after heart attacks include arrhythmias (abnormal heart rhythms), heart failure, sudden cardiac arrest, heart valve problems, and depression, according to the Cleveland Clinic.
What Is Cardiac Arrest?
Sudden cardiac arrest is a problem with the heart’s electrical system, and it usually strikes without warning. “The heart suddenly stops beating or develops a chaotic beating and no blood is pumped to the rest of the body,” says Batiste. The mortality rate for out-of-hospital cardiac arrests is between 70 and 90 percent, according to the CDC. Survival is possible if treated within minutes using CPR, a defibrillator, or chest compressions, until emergency workers arrive. Survivors of cardiac arrest may have nerve or brain damage.
Sometimes heart attacks can trigger cardiac arrest, but cardiac arrest does not cause heart attacks, says Batiste.
Symptoms of a Heart Attack
The earliest sign of a heart attack might be recurrent chest pain or pressure that's triggered by activity and relieved by rest, according to the Mayo Clinic. Symptoms often start slowly and persist for hours, days, or even weeks before a heart attack. The most common symptoms include:
- Pain or discomfort—that lasts for more than a few minutes or goes away and comes back—in the chest, jaw, neck, back, or abdomen, one or both arms or shoulders
- Breaking out in a cold sweat
- Nausea or vomiting
- Lightheadedness; feeling weak or faint
- Unusual or unexplained tiredness
- Shortness of breath
About 1 in 5 heart attacks occur silently—i.e., without the person’s awareness—according to the Centers for Disease Control.
Symptoms of Cardiac Arrest
Sometimes cardiac arrest is preceded by chest discomfort, shortness of breath, weakness, or heart palpitations. However, typically there is no warning, so the first signs are drastic:
- Loss of responsiveness
- Collapse
- No pulse or breathing
For both heart attack and cardiac arrest, survival odds increase the faster that treatment can be administered. Call 911 immediately. Emergency medical services can begin treatment up to an hour sooner than if you drive to the ER, the American Heart Association notes.. Patients who arrive by ambulance usually receive faster treatment at the hospital.
Risk Factors and Causes
The main cause of heart attack is coronary artery disease. Over time, a buildup of fatty deposits, called plaques, narrow the arteries and impede blood flow to the heart.
Cardiac arrest typically occurs in a heart that has been damaged by an existing condition, such as coronary heart disease or heart attack. Risk factors for sudden cardiac arrest include:
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
- Obesity
- Poor diet (see “Foods to Avoid,” below)
- Sedentary lifestyle
- Excessive alcohol use
- Recreational drug use
Preventing Heart Attack and Cardiac Arrest
According to the Harvard School of Public Health, following a healthy lifestyle may prevent 80 percent of sudden cardiac deaths and 72 percent of premature deaths related to heart disease. “The core to lifestyle change includes what we eat, how we move, and how we rest,” says Batiste. “Each component is essential in achieving heart health and living our best lives.”
The American Heart Association developed seven metrics for heart health. In a study of more than 7,000 people, those who met five or more of these metrics lowered their risk of heart-related death by 88 percent compared with people who met none of these ideal metrics.
- Smoking cessation
- Achieving an ideal body weight
- Maintaining normal blood sugar
- Maintaining normal blood pressure
- Achieving an ideal lipid profile
- Exercise
- Eating a plant-based diet
Exercise
Exercise strengthens the heart muscle and keeps the arteries flexible to help maintain healthy blood flow. Exercise lowers the risk of heart disease and contributing factors such as obesity, high blood pressure, high cholesterol, and diabetes.
The American Heart Association recommends working up to at least 150 minutes a week of moderate-intensity aerobic activity (like walking) or 75 minutes of vigorous-intensity aerobic activity (like running). One study in The BMJ found that regular exercise of brisk walking correlated to an over 50 percent reduction in coronary events. Another study found that, compared with active patients, inactive coronary artery disease patients had 2.4-fold increased risk for sudden cardiac death.
Sleep
A study in the Journal of the American College of Cardiology found people who slept fewer than six hours a night had a 20 percent higher risk of heart attack than those who slept six to nine hours. “Taking time to rest and sleep is important to prevent heart attacks and strokes,” says Batiste.
Foods to Avoid
Eating a diet high in saturated fats, trans fat, cholesterol, and sodium has been linked to heart disease. Research suggests that it is impactful to limit inflammatory foods (meats, fried foods, processed foods, sweets, and sugar-sweetened beverages). “What we eat matters,” says Batiste. In a 2021 study published in the Journal of the American Heart Association, people who ate a diet high in fats, fried foods, processed meats, and sugary drinks had a 46 percent increased risk of sudden cardiac death.
Drinking too much alcohol can raise blood pressure levels and increase levels of triglycerides, which increase the risk for heart disease. The American Heart Association recommends that women have no more than one drink a day and men have no more than two drinks a day.
Foods to Eat
“Heart health starts with what you choose to put in your mouth,” says Batiste. “Choosing a whole-food, plant-based diet has been proven to improve heart health.” Build your plate around plant foods, including vegetables, whole grains, legumes, nuts, and seeds.
In the Journal of the American Heart Association study cited above, those who ate a plant-heavy diet had a 26 percent lower risk of sudden cardiac death. Another 2021 study in the Journal of the American Heart Association, found that those who ate a plant-centered diet in young adulthood, between ages 18 and 30, were 52 percent less likely to develop cardiovascular disease during about 30 years of follow-up.
Plant-based diets help people improve their weight, cholesterol, and blood pressure and lower the risk of diabetes—all of which lower the risk of heart attack and cardiac arrest. “A journey to a better you begins with the first bite,” says Batiste. “It doesn’t matter how you start—1 percent or 100 percent—just start. If you really want heart health, it has to become your North Star.”
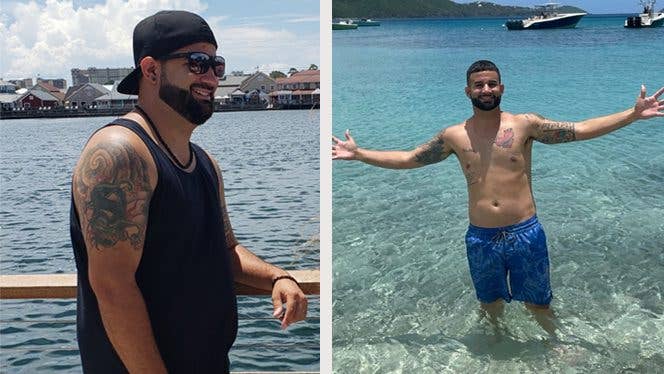
Stories of Survival
Read on for inspirational firsthand accounts from people who survived cardiac arrest or heart attack, made lifestyle adjustments, and improved their health overall.
- The Heart Attack That Could Have Killed Me Made Me Stronger
- After Heart Attack, I'm Thriving on a Plant-Based Diet
- I Went Vegan After Cardiac Arrest Nearly Killed Me
- I Fully Recovered From a Heart Attack in 3 Months of Eating Plants
- Post Heart Attack, Living It Up at 84 on a Plant-Based Diet
- How This Doctor Reversed Heart Disease After a Heart Attack at 40
- From Heart Attack to Healthy Heart in Two Years With No Meds
- After a Heart Attack, I Changed My Diet, Shocked My Cardiologist, and Avoided Bypass Surgery
- Barely Survived a Massive Heart Attack … I Never Want Another One!
To learn more about a whole-food, plant-based diet, visit our Plant-Based Primer. For meal-planning support, check out Forks Meal Planner, FOK’s easy weekly meal-planning tool to keep you on a healthy plant-based path.
Related News
Try Our Top-RatedMeal Planner Free

Forks Meal Planner takes the hard work out of making nutritious meals the whole family will enjoy.
SAVE $200 ON OUR ULTIMATE COURSE

Join our best-selling course at a new lower price!