HEALTH TOPICS
Metabolic Syndrome and Diet: Here’s What You Need To Know
Affecting 1 in 3 adults, metabolic syndrome is fairly common in the United States. A constellation of conditions, it puts people at higher risk of cardiovascular disease, diabetes, stroke, and other serious health problems, like atherosclerosis. The good news? Simple lifestyle changes and healthy habits can reduce that risk and may even be able to reverse the damage that has already been done.
What Is Metabolic Syndrome?
Doctors have long been interested in uncovering a connection between obesity, diabetes, and heart disease. Metabolic syndrome, also known as Syndrome X or insulin resistance syndrome, emerged as a way to describe shared underlying characteristics.
Metabolic Syndrome Symptoms
You may be diagnosed with metabolic syndrome if you have at least three of the five following conditions.
- A large waist circumference: You have an “apple-shaped” body, or your waist circumference measures greater than 35 inches for women or greater than 40 inches for men.
- High blood glucose (sugar): Your blood sugar measures 100 mg/dL or more, or you take medicine for high blood glucose.
- Low levels of HDL (“good”) cholesterol: Your HDL levels are less than 40 mg/dL for men or less than 50 mg/dL for women.
- High levels of triglycerides: Your triglyceride levels measure 150 mg/dL or more, or you take medicine for high triglycerides.
- High blood pressure: Your blood pressure measures 130/85 mmHg or more, or you take medicine for hypertension.
Risk Factors
A variety of traits, conditions, and lifestyle behaviors put you at greater risk of developing metabolic syndrome. The following may occur on their own or in combination with other risk factors.
- Excessive fat in and around the abdomen
- Inactivity (less than the recommended 150 minutes per week of exercise)
- Too much or too little sleep (more than 10 hours or less than six hours)
- Smoking and/or heavy alcohol consumption
- Age: Your risk increases as you get older.
- Gender: Men are at a greater risk than women, although women are more likely to have low HDL.
- Ethnicity: Metabolic syndrome is most prevalent among Hispanic adults.
- A family history of diabetes or metabolic syndrome
- Insulin resistance, which occurs when cells don't respond normally to insulin
- Polycystic ovary syndrome, a condition that causes cysts to grow on the ovaries
- Chemotherapy: Women treated with chemotherapy before or after breast cancer surgery are at a higher risk.
How Does Diet Affect Metabolic Syndrome?
“Metabolic syndrome is certainly very much impacted by diet,” says Nicole Harkin, MD, FACC, founder of Whole Heart Cardiology. “The central component to it is weight gain which is often created by a combination of genetic factors, a sedentary lifestyle, and then dietary factors that really go into developing insulin resistance and a body weight that's above ideal.”
A primary culprit, she says, is the standard American diet, which tends to be rich in highly processed foods.
A 2021 study published in Liver International investigated the connection between ultra-processed foods and metabolic syndrome. A total of 789 male and female participants (59 years old on average) received a food frequency questionnaire, an abdominal ultrasound, body measurements, blood pressure measurements, and fasting blood tests. Researchers found that eating more ultra-processed foods was associated with higher odds for metabolic syndrome and its components—hypertension, hypertriglyceridemia, and low HDL.
Another culprit, according to at least two studies, is the high consumption of red meat and processed meats.
On the flip side, evidence shows that a whole-food, plant-based diet can play a protective role against metabolic syndrome. Not only is it low in saturated fat; it’s also high in fiber, which could be effective in the management of metabolic syndrome for its ability to control body weight through its effect on satiety (among other health benefits). And research indicates that eating greater quantities of fruits and vegetables is associated with a lower risk of metabolic syndrome.
How to Reverse Metabolic Syndrome
“While [metabolic syndrome] might sound like a scary diagnosis, it's definitely something that you can turn around with lifestyle changes,” says Harkin.
A healthy diet and regular exercise are keys to doing just that, according to a 2007 study published in the Journal of General Internal Medicine.
Researchers divided 335 metabolic syndrome patients aged 45 to 64 in northwest Italy into an intervention group and a control group. The intervention group reduced saturated fat intake and increased polyunsaturated fat and fiber intake, along with exercise levels. After 12 months, researchers saw weight, waist circumference, high-sensitivity C-reactive protein (a marker of inflammation), and most metabolic syndrome components decrease in the intervention group and increase in the control group.
“Getting an adequate amount of exercise is a great part of preventing and reversing metabolic syndrome,” says Harkin.
And it doesn’t need to be vigorous exercise, which may be especially challenging for overweight or more sedentary individuals. Instead, according to a 2007 study published in the American Journal of Cardiology, even moderate exercise, such as walking about 12 miles per week, can sufficiently improve metabolic syndrome. Alternately, the American Heart Association recommends 30 to 60 minutes per day of moderate-intensity physical activity supplemented by two days per week of resistance training.
“If you lose somewhere between just 5–10% of your body weight, that can really improve your insulin sensitivity and reverse some of the cardiometabolic abnormalities that we see in association with metabolic syndrome,” says Harkin.
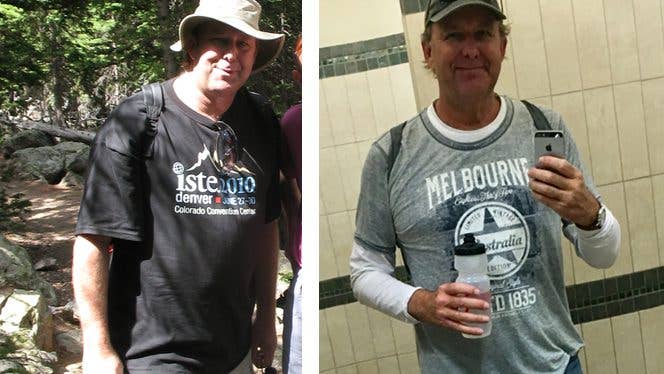
Real-Life Success Stories
By adopting a healthier lifestyle, it's possible to avoid and even reverse metabolic syndrome and its risk factors. For inspiration, check out the following first-person testimonials from individuals who have—with the help of a whole-food, plant-based diet—done just that:
- I’m Reversing Metabolic Syndrome on a Plant-Based Diet
- I’ve Normalized Sky-High Triglycerides and Begun Reversing Kidney Disease in Just 12 Weeks
- What a Plant-Based Diet Did to My Cholesterol, Blood Sugar, and Triglycerides
- From Cheese-Loving Vegetarian with Sky-High Blood Pressure to Whole-Food, Plant-Based and Healthy
- What Giving Up Meat, Dairy, and Processed Foods Did for My BMI, Blood Pressure, and Cholesterol
To learn more about a whole-food, plant-based diet, visit our Plant-Based Primer. For meal-planning support, check out Forks Meal Planner, FOK’s easy weekly meal-planning tool to keep you on a healthy plant-based path.
About the Author

About the Author
Lindsay Morris
Lindsay Morris is a Los Angeles-based writer whose work has appeared in publications including Shape, Natural Health, Chicago Tribune, and Women’s Adventure. A graduate of Marquette University, she enjoys hiking, camping, and baking home-milled bread.
SIMILAR ARTICLES
Join our mailing list
Get free recipes and the latest info on living a happy, healthy plant-based lifestyle.
By providing your email address, you consent to receive newsletter emails from Forks Over Knives. We value your privacy and will keep your email address safe. You may unsubscribe from our emails at any time.