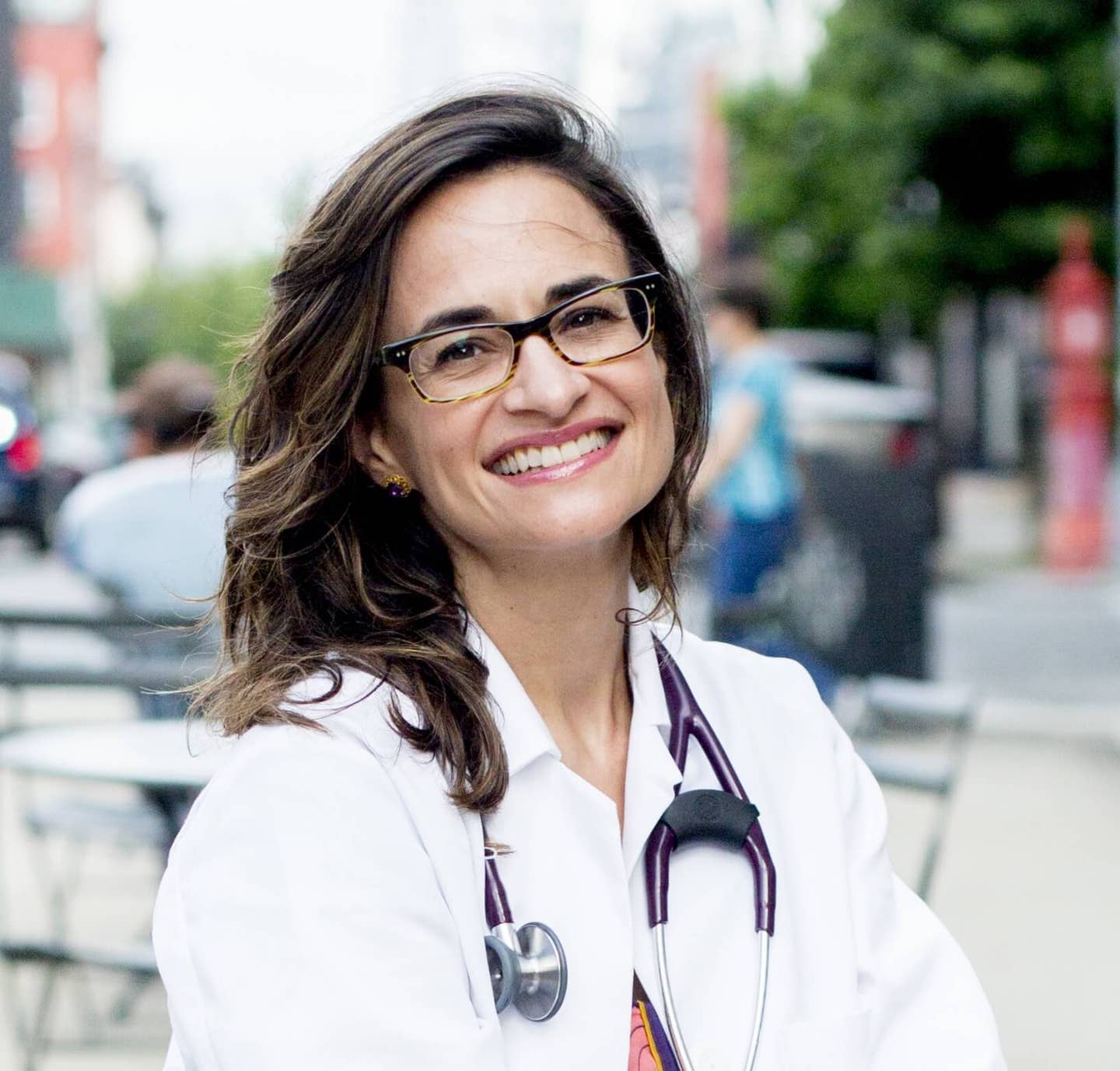
I have many patients with type 2 diabetes and prediabetes in my internal medicine practice. When I ask what foods they think they should limit, the majority answer “carbs.” To their surprise, I tell them that I actually recommend a high-carb diet—one based in whole- or minimally processed plant foods. Here’s why:
People eating high-carb, high-fiber diets enjoy exceptional protection from type 2 diabetes. The Adventist Health Study 2 showed that among nearly 61,000 people, vegans—whose diets are typically high in carbohydrate-rich foods—had half the rate of diabetes compared to non-vegetarians, even after accounting for differences in body weight. It is notable that the non-vegetarians in this study ate red meat and poultry relatively infrequently, suggesting that even small increases in meat consumption disproportionately increase the risk of type 2 diabetes.
Other studies from the Adventist group show similar trends. Among 41,387 Adventists followed for two years, vegans had a 62 percent lower risk of developing diabetes compared to omnivores. And among 8,401 Adventists followed for 17 years, eating meat just once a week was linked to a dramatic 74 percent higher risk of diabetes! Both studies adjusted for body weight and other lifestyle variables.
Moreover, in one of the largest studies of plant-based eating patterns to date, people eating a diet emphasizing whole, unprocessed plant foods had a 34 percent lower chance of developing type 2 diabetes in the long term compared with those whose diets were rich in animal products and/or processed foods. However, those eating a plant-based diet high in less-healthy foods such as fruit juices, sweetened beverages, fried potatoes, chips, refined grains, and desserts experienced a 16 percent increased risk of diabetes, highlighting the importance of choosing healthy plant foods.
A high-carb, high-fiber diet can lower insulin resistance. Insulin resistance is the root problem in prediabetes and type 2 diabetes. In people with insulin resistance, sugar in the blood doesn't enter our cells as easily it should, and the liver produces too much sugar. Over time, this can result in type 2 diabetes.
The causes of insulin resistance are complex, but the key players are inflammation, excess dietary fats and calories, unhealthy weight gain, and the buildup of fats inside our muscle and liver cells. Here’s where much of the confusion about carbs begins: In people with insulin resistance, carbohydrate-rich foods—such as fruit—can cause spikes in blood sugar because sugar can’t enter the cells properly. This leads people to believe that the fruit is somehow at fault, and that they should limit all carbohydrate-rich foods to keep their blood sugar lower.
Quite the opposite! When we avoid healthy carbs, we are masking the real issue. A whole-foods, plant-based diet actually treats the underlying cause of insulin resistance because it lowers inflammation, promotes a healthy body weight, and reduces the buildup of fats inside our cells. When we become less insulin resistant, our blood sugar doesn’t go up as high when we eat carbohydrate-rich foods. That is a true test of whether a diet reverses insulin resistance instead of simply treating the symptom of high blood sugar.
But what about that piece of fruit? Does fruit cause diabetes? Actually, large studies have linked fruit consumption to lower rates of type 2 diabetes, as well as a reduced risk of diabetes complications and premature death in people who already have diabetes. Overall, whole grains (such as oats, barley, brown rice, and whole wheat) are the type of food that is most consistently protective against type 2 diabetes, while processed meat (which contains almost no carbohydrates) increases diabetes risk the most—just one serving per day raises the risk by 37 percent!
High-carb, plant-based diets are effective for treating, and in some cases reversing, type 2 diabetes. Randomized clinical trials show that a fully plant-based diet that is high in carbohydrates and fiber and low in fat can lower glycosylated hemoglobin (a measure of average blood sugar), reduce the need for medications, help people lose excess weight, and even lower blood cholesterol more than a conventional diet based on American Diabetes Association guidelines. Notably, plant-based patients in these trials were not asked to measure portions, count carbs, or tally their calories. They just ate healthier foods! A 2014 review of vegetarian diets for the treatment of type 2 diabetes confirmed significant reductions in blood sugar compared to standard diets.
Whole-food, plant-based, high-carbohydrate diets typically exclude nutrients and foods that have been associated with diabetes risk, including animal protein, saturated animal fats, refined grains, and sugar-sweetened beverages. They emphasize unprocessed plant foods, which are naturally rich in fiber, antioxidants, and phytonutrients—substances that reduce inflammation and promote a healthy body weight.
A high-carb, plant-based diet can prevent and treat cardiovascular disease and other complications of diabetes. Plant-based diets have been shown to prevent and reverse cardiovascular disease, the leading cause of death in those with type 2 diabetes. They also lower blood cholesterol, blood pressure, and inflammation, major risk factors for cardiovascular disease. A growing body of scientific literature shows that plant-based diets may be helpful in delaying the progression of chronic kidney disease, a common complication of diabetes. A plant-based diet may lessen the pain of diabetic neuropathy, a debilitating nerve-related condition in diabetes. Finally, plant-based diets are effective for weight loss, which further improves diabetes control.
Eating more healthful, carb-rich foods tends to crowd out disease-promoting foods. Added sugars, animal fats, animal protein, and white flour and other refined grains all increase our risk of chronic disease and, in the case of animal protein, even premature death. Animal foods in particular contain higher levels of saturated fat; heme iron; advanced glycation end products; and in the case of processed meats, nitrate and nitrite preservatives. They also stimulate our gut bacteria to make a harmful compound called TMAO. All of these substances promote insulin resistance and other health risks. When you focus on beans, lentils, peas, fruits, vegetables, and whole grains, you not only improve your diabetes or risk of diabetes, but you stack the odds in favor of optimal long-term health.
My patients with prediabetes and diabetes who adopt a high-carbohydrate, high-fiber, WFPB diet typically experience lower blood sugars and lower cholesterol, as well as weight loss if they are overweight. They have been able to reduce medications in many cases. I’ve seen this approach work well, and I’m certainly not the only one recommending it: Mainstream diabetes organizations have recognized the value of a plant-based diet for diabetes. In their 2018 guidelines, the American Association of Clinical Endocrinologists (AACE) recommends a plant-based diet as the preferred eating pattern for patients with type 2 diabetes, and the American Diabetes Association advises that a plant-based diet is a healthful option for patients with type 2 diabetes.
If you have diabetes, be sure to work closely with your health care provider if you change your diet, as any medications you are taking may require adjustment. For practical information on how to adopt a plant-based diet for diabetes, check out resources such as the Physicians Committee for Responsible Medicine and Mastering Diabetes.
Ready to get started? Check out Forks Meal Planner, FOK’s easy weekly meal-planning tool to keep you on a healthy plant-based path. To learn more about a whole-food, plant-based diet, visit our Plant-Based Primer.
Related News
Try Our Top-RatedMeal Planner Free

Forks Meal Planner takes the hard work out of making nutritious meals the whole family will enjoy.
SAVE $200 ON OUR ULTIMATE COURSE

Join our best-selling course at a new lower price!